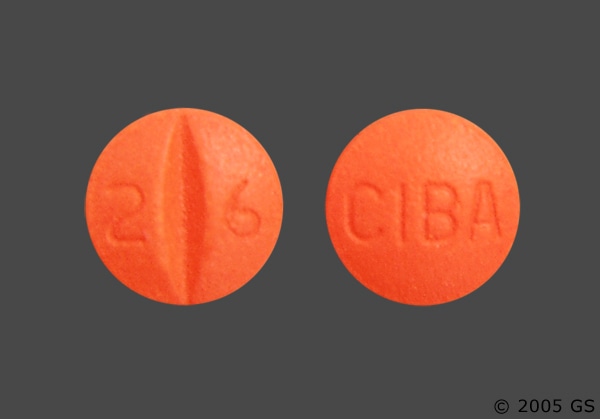
Maprotiline | Ludiomil
Maprotiline hydrochloride tab lets are indicated for the treatment of depressive illness in patients with depressive neurosis (dysthymic disorder) and manic depressive illness, depressed type (major depressive disorder). Maprotiline is also effective for the relief of anxiety associated with depression.
A single daily dose is an alternative to divided daily doses. Therapeutic effects are sometimes seen within 3 to 7 days, although as long as 2 to 3 weeks are usually necessary. Initial Adult Dosage: An initial dosage of 75 mg daily is suggested for outpatients with mild to moderate depression. However, in some patients, particularly the elderly, an initial dosage of 25 mg daily may be used. Because of the long half-life of maprotiline, the initial dosage should be maintained for 2 weeks. The dos age may then be increased gradually in 25 mg increments as required and tolerated. In most outpatients a maximum dose of 150 mg daily will result in therapeutic efficacy. It is recommended that this dose not be exceeded except in the most severely de pressed patients. In such patients, dos age may be gradually in creased to a maximum of 225 mg. More severely depressed, hospitalized patients should be given an initial daily dose of 100 mg to 150 mg which may be gradually increased as required and tolerated. Most hospitalized patients with moderate to severe depression respond to a daily dose of 150 mg although dosages as high as 225 mg may be re quired in some cases. Daily dosage of 225 mg should not be exceeded.
—–INDICATIONS AND USAGE—–
- See description above.
—–DOSAGE AND ADMINISTRATION—–
- See description above.
—–CONTRAINDICATIONS—–
- Maprotiline hydrochloride tab lets are contraindicated in patients hypersensitive to maprotiline and in patients with known or suspected seizure disorders. It should not be given concomitantly with monoamine oxidase (MAO) inhibitors. A minimum of 14 days should be allowed to elapse after discontinuation of MAO inhibitors before treatment with maprotiline is initiated. Effects should be monitored with gradual increase in dosage until optimum response is achieved. The drug is not recommended for use during the acute phase of myocardial infarction.
—–WARNINGS—–
- Clinical Worsening and Suicide Risk: Patients with major depressive disorder (MDD), both adult and pediatric, may experience worsening of their depression and/or the emergence of suicidal ideation and behavior (suicidality) or unusual changes in behavior, whether or not they are taking antidepressant medications, and this risk may persist until significant remission occurs. Suicide is a known risk of depression and certain other psychiatric disorders, and these disorders themselves are the strongest predictors of suicide. There has been a long-standing concern, however, that antidepressants may have a role in inducing worsening of depression and the emergence of suicidality in certain patients during the early phases of treatment. Pooled analyses of shortterm placebo-controlled trials of antidepressant drugs (SSRIs and others) showed that these drugs increase the risk of suicidal thinking and behavior (suicidality) in children, adolescents, and young adults (ages 18-24) with major depressive disorder (MDD) and other psychiatric disorders. Short-term studies did not show an increase in the risk of suicidality with antidepressants compared to placebo in adults beyond age 24; there was a reduction with antidepressants compared to placebo in adults aged 65 and older.
- Screening Patients for Bipolar Disorder: A major depressive episode may be the initial presentation of bipolar disorder. It is generally believed (though not established in controlled trials) that treating such an episode with an antidepressant alone may increase the likelihood of precipitation of a mixed/manic episode in patients at risk for bipolar disorder. Whether any of the symptoms described above represent such a conversion is unknown. However, prior to initiating treatment with an antidepressant, patients with depressive symptoms should be adequately screened to determine if they are at risk for bipolar disorder; such screening should include a detailed psychiatric history, including a family history of suicide, bipolar disorder, and depression. It should be noted that maprotiline is not approved for use in treating bipolar depression.
- Seizures have been associated with the use of maprotiline. Most of the seizures have occurred in patients without a known history of seizures. However, in some of these cases, other confounding factors were present, including concomitant medications known to lower the seizure threshold, rapid escalation of the dosage of maprotiline, and dosage that exceeded the recommended therapeutic range. The incidence of direct re ports is less than 1/10 of 1%. The risk of seizures may be increased when maprotiline is taken concomitantly with phenothiazines, when the dos age of benzodiazepines is rapidly tapered in patients receiving maprotiline or when the recommended dosage of maprotiline hydrochloride is exceeded. While a cause and effect relationship has not been established, the risk of seizures in patients treated with maprotiline may be reduced by (1) initiating therapy at a low dos age, (2) maintaining the initial dosage for 2 weeks before raising it gradually in small increments as necessitated by the long half-life of maprotiline (average 51 hours), and (3) keeping the dos age at the minimally effective level during maintenance therapy. (See DOSAGE AND ADMINISTRATION.)
—–PRECAUTIONS—–
- General: The possibility of suicide in seriously depressed patients is inherent in their illness and may persist until significant remission occurs. Therefore, patients must be carefully supervised during all phases of treatment with maprotiline, and prescriptions should be writ ten for the smallest number of tablets consistent with good patient management. Hypomanic or manic episodes have been known to occur in some patients taking tricyclic antidepressant drugs, particularly in patients with cyclic disorders. Such occurrences have also been noted, rarely, with maprotiline. Prior to elective surgery, maprotiline should be discontinued for as long as clinically feasible, since little is known about the interaction between maprotiline and general anesthetics. Maprotiline should be ad ministered with caution in patients with history of urinary retention, or history of narrow angle glaucoma because of the drug’s anticholinergic properties.
- Information for Patients: Prescribers or other health professionals should inform patients, their families, and their caregivers about the benefits and risks associated with treatment with maprotiline and should counsel them in its appropriate use. A patient Medication Guide about “Antidepressant Medicines, Depression and other Serious Mental Illness and Suicidal Thoughts or Actions” is available for maprotiline. The prescriber or health professional should instruct patients, their families, and their caregivers to read the Medication Guide and should assist them in understanding its contents. Patients should be given the opportunity to discuss the contents of the Medication Guide and to obtain answers to any questions they may have. The complete text of the Medication Guide is reprinted at the end of this document. Patients should be advised of the following issues and asked to alert their prescriber if these occur while taking maprotiline. Patients should be advised that taking maprotiline can cause mild pupillary dilation, which in susceptible individuals, can lead to an episode of angle-closure glaucoma. Pre-existing glaucoma is almost always open-angle glaucoma because angle-closure glaucoma, when diagnosed, can be treated definitively with iridectomy. Open-angle glaucoma is not a risk factor for angle-closure glaucoma. Patients may wish to be examined to determine whether they are susceptible to angle-closure, and have a prophylactic procedure (e.g., iridectomy), if they are susceptible.
- Carcinogenesis, Mutagenesis, Impairment of Fertility: Carcinogenicity and chronic toxicity studies have been con ducted in laboratory rats and dogs. No drug- or dose-related occurrence of carcinogenesis was evident in rats receiving daily oral doses up to 60 mg/kg of maprotiline hydro chloride for 18 months or in dogs receiving daily oral doses up to 30 mg/kg of maprotiline hydrochloride for one year. In addition, no evidence of mutagenic activity was found in off spring of female mice mated with males treated with up to 60 times the maximum daily human dose.
—–ADVERSE REACTIONS—–
The following adverse reactions have been noted with maprotiline and are generally similar to those observed with tricyclic antidepressants.
- Cardiovascular: Rare occurrences of hypotension, hypertension, tachycardia, palpitation, arrhythmia, heart block, and syncope have been re ported with maprotiline.
- Psychiatric: Nervousness (6%), anxiety (3%), insomnia (2%), and agitation (2%); rarely, confusional states (especially in the elderly), hallucinations, disorientation, delusions, restlessness, nightmares, hypomania, mania, exacerbation of psychosis, de crease in memory, and feelings of unreality.
- Neurological: Drowsiness (16%), dizziness (8%), tremor (3%), and, rarely, numb ness, tingling, motor hyperactivity, akathisia, seizures, EEG alterations, tinnitus, extrapyramidal symptoms, ataxia, and dysarthria.
- Anticholinergic: Dry mouth (22%), constipation (6%), and blurred vision (4%); rarely, accommodation disturbances, mydriasis, urinary retention, and delayed micturition.
- Allergic: Rare instances of skin rash, petechiae, itching, photosensitization, edema, and drug fever. Gastrointestinal: Nausea (2%) and, rarely, vomiting, epigastric distress, diarrhea, bitter taste, abdominal cramps and dysphagia.
- Endocrine: Rare instances of in creased or decreased libido, impotence, and elevation or depression of blood sugar levels.
- Other: Weakness and fatigue (4%) and headache (4%); rarely, altered liver function, jaundice, weight loss or gain, excessive perspiration, flushing, urinary frequency, in creased salivation, nasal congestion and alopecia. Note: Although there have been only isolated reports of the following adverse reactions with maprotiline, its pharmacologic similarity to tricyclic antidepressants requires that each reaction be considered when administering maprotiline. — Bone marrow depression, including agranulocytosis, eosinophilia, purpura, and thrombocytopenia, myocardial infarction, stroke, peripheral neuropathy, sublingualadenitis, black tongue, stomatitis, paralyticileus, gynecomastia in the male, breast enlargement and galactorrhea in the female, and testicular swelling.
- Postintroduction Reports: Voluntary reports of adverse events temporally associated with maprotiline that have been received since market introduction and that may have no casual relationship with the drug include the following: interstitial pneumonitis which were in some cases associated with eosinophilia and increased liver enzymes, Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis.
—–DRUG INTERACTIONS—–
Close super vision and careful ad justment of dosage are required when administering maprotiline concomitantly with anticholinergic or sympathomimetic drugs because of the possibility of additive atropine like effects. Concurrent administration of maprotiline with electro shock therapy should be a voided because of the lack of experience in this area. Caution should be exercised when administering ma protiline to hyperthyroid patients or those on thyroid medication because of the possibility of enhanced potential for cardiovascular toxicity of maprotiline. Maprotiline should be used with caution in patients receiving guanethidine or similar agents since it may block the pharmacologic effects of these drugs. The risk of seizures may be increased when maprotiline is taken concomitantly with phenothiazines or when the dos age of benzodiazepines is rap idly tapered in patients receiving maprotiline. Because of the pharmacologic similarity of maprotiline hydrochloride to the tricyclic antidepressants, the plasma concentration of maprotiline may be increased when the drug is given concomitantly with hepatic enzyme inhibitors (e.g., cimetidine, fluoxetine) and de – creased by concomitant administration with hepatic enzyme inducers (e.g., barbiturates, phenytoin), as has occurred with tricyclic antidepressants. Adjustment of the dos age of maprotiline hydrochloride may therefore be necessary in such cases.

